Liver cancer is one of the deadliest forms of the disease and is on the rise both globally and domestically. While CRI-funded scientists work relentlessly to research immunotherapy solutions that can lift patient outcomes, a prevalence of previous hepatitis infection among patients and immune cells that actually enable liver tumors complicates the search for a cure.
Liver cancer is the 1st known cancer with a viral onset, with 80% of patients previously diagnosed with hepatitis.
5 Fast Facts About Liver Cancer

1. Liver cancer has a five-year survival rate of 17 percent. What concerns Seth Coffelt, PhD, professor of cancer immunology at the University of Glasgow in the U.K. and CRI CLIP Investigator, is that most liver cancer patients do not respond to current immunotherapies. Part of the problem is a type of immune cell, the gamma delta T cell, which lives inside the liver. These cells actually enable tumor growth instead of fighting cancer.
“Our immune system has evolved to protect us from invaders and abnormalities from outside our bodies; however, liver cancers have the ability to turn off these responses and instead trigger immune cells to assist their growth,” Dr. Coffelt explained. He stressed that more research is needed to understand the mechanisms of liver cancer growth to create tailored treatments for patients.
2. It is the first known cancer that has a viral onset. Hepatitis is responsible for the vast majority of cases, around 80 percent. There is a preventative vaccine for hepatitis B (HBV), but not for hepatitis C (HCV). HBV and HCV can cause scarring, and in an effort to mend and replace liver tissue, faulty DNA replication and liver cell division can lead to cancer. Patients with a history of hepatitis infection might not be viable candidates for liver cancer immunotherapy treatment because of the risk for damaging healthy liver cells.
3. There are a wide variety of liver cancer symptoms, but they include unintended weight loss, decrease in appetite, nausea, dark urine, and more. Certain conditions, such as chronic HCV, non-alcoholic fatty liver disease, and others can increase the risk of liver cancer. Blood tests, CT scans, and MRI scans are all widely used as screening options.
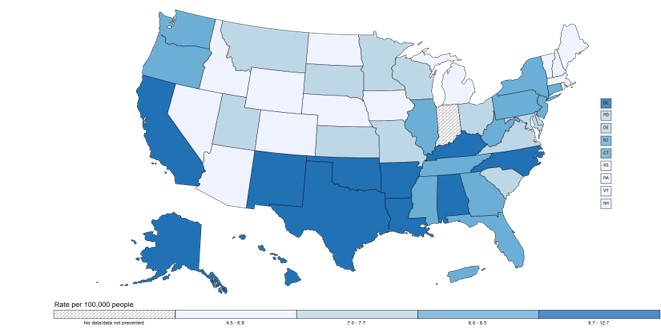
4. Liver cancer rates vary based on several factors. Geographically in the U.S., rates are highest in the south and the west coast, per the U.S. Centers for Disease Control and Prevention (CDC). Furthermore, its rate among men is more than twice as high than for women, and Hispanic people are more likely to receive a liver cancer diagnosis than any other ethnic group.
Rate of New Cancers in the United States, 2021. Liver and Intrahepatic Bile Duct, All Ages, All Races and Ethnicities, Male and Female
5. There are three main types of liver cancer:
- Hepatocellular carcinoma (HCC) occurs as a liver tumor. Dr. Coffelt said that it is the fourth-largest cause of cancer deaths globally. When HCC spreads, the standard of care is to treat the patient with immunotherapy via a checkpoint inhibitor combined with a targeted antibody to unleash the immune system’s full power to stop the cancer cells’ harmful activity.
- Cholangiocarcinoma, a cancer of the bile duct, the canals that connect several organs of the digestive system. While it is a rare cancer, its five-year survival rate sits at two percent.
- Hepatoblastoma most commonly occurs in children younger than four years old but is very rare and usually does not spread outside the liver. Genetic conditions and a low birth weight are possible indicators of a greater risk for this disease.
The Arc of Discovery: CRI’s Impact on Liver Cancer Immunotherapy

CRI scientists who work hard to combat liver cancer do so with focused, detailed research that emphasizes the journey from initial discovery to therapeutic impact. Nadia Guerra, PhD, associate professor and head of the Inflammation and Cancer Immunity Lab at Imperial College London, is a CRI-Esther M. Baird Technology Impact Award Investigator who aims to implement a novel, multidisciplinary project. Dr. Guerra is using multiplexed nanobiosensors, which are chemical sensors that translate signals into quantifiable data, to create a fingerprinting method that can detect genetic and protein markers for cancer type and disease stage.
Dr. Guerra’s biosensor platform will enable earlier and more accurate cancer detection, it will also help in determining how well the treatment works and if there are any side effects in real-time. This will in turn help in tailoring treatment plans based on patient responses to specific treatments. In February of 2024, she co-authored a research paper that detailed how clusters of laboratory-produced proteins called monoclonal antibodies combined with multi-receptor stimulation can maximize the impact of Natural Killer T cells that attack cancer cells.

Additionally, Marina Baretti, MD, assistant professor of oncology at Johns Hopkins University School of Medicine and CRI Clinical Innovator, focused her research on how the changes in genetic code are the driving force behind fibrolamellar hepatocellular carcinoma (FLC), a rare and deadly form of liver cancer. Dr. Baretti has discovered that targeting glutamine metabolism can enhance the efficiency of immunotherapy. She is now leading a clinical trial that combines a drug targeting glutamine metabolism with the immune checkpoint inhibitor durvalumab to treat FLC patients. In July of 2024, she was the senior author of a research paper that highlighted the need for further surveillance of FLC patients to address the possibility of cancer recurrence.
Immunotherapy holds the promise for advancements in all cancers, but some present a greater challenge to scientific researchers than others. Dr. Coffelt expressed that immunologists have to target the very immune cells that should harm cancer, not aid it, to benefit liver cancer patients. He remained hopeful that future therapies would be able to accomplish this noble task. With innovative and results-driven scientists like Drs. Coffelt, Guerra, and Baretti hard at work to thwart this formidable disease, we march ever-closer to a world immune to cancer.
